Life Blood
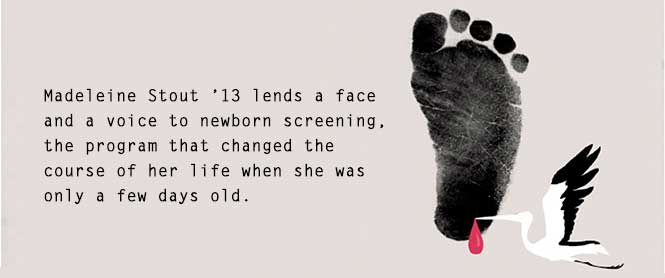
Dr. Marvin Mitchell actually met Madeleine Stout ’13 in person last fall, but he first encountered her twenty-three years ago in the form of one of the thousands of blood droplets that pass each week through the Boston laboratory at the New England Newborn Screening Program, which he directed at the time. The program screens for diseases not readily apparent to a parent’s or a physician’s gaze that can do great harm if not found and treated within the first days of life. Though the technical challenges in processing and analyzing approximately 150,000 specimens a year can be daunting, “one has to always be aware that each one of these little blood spots is a baby,” says Mitchell.
Just hours after her birth, Stout’s blood was taken from a pinprick on her heel per laboratory protocol. The sample was deposited on a piece of filter paper, dried, and sent to Mitchell’s lab. Stout was then identified as among the approximately one in 2,000 infants flagged in New England each year for congenital hypothyroidism, a very serious disorder that stems from a malfunctioning, or, in Stout’s case, absent thyroid gland. If untreated the condition can lead to physical malformations and severe brain damage. “The severest form of the disorder,” says Mitchell, “results in irreversible neurological disease with IQs well below eighty-five.” But if the infant is immediately administered the vital hormones her body is not producing on its own, the damage can be averted and she can grow up symptom free.
 The occasion of Mitchell and Stout’s meeting was a celebration at the Massachusetts State House for the fiftieth anniversary of mandatory newborn screening for phenylketonuria, or PKU, a deficiency in the body’s ability to metabolize certain foods. If not addressed quickly, PKU can result in stunted growth, microcephaly, and brain damage. In the early 1970s Mitchell was at the New England Newborn Screening Program when Jean Dussault, a Canadian physician who became a close personal friend, realized that the approach to early detection of PKU could be applied to congenital hypothyroidism. The disease had frustrated doctors for years because of the knowledge that early detection and treatment could head off symptoms before, to use Mitchell’s word, they “blossomed.” Congenital hypothyroidism was added to the screening protocol later that decade.
The occasion of Mitchell and Stout’s meeting was a celebration at the Massachusetts State House for the fiftieth anniversary of mandatory newborn screening for phenylketonuria, or PKU, a deficiency in the body’s ability to metabolize certain foods. If not addressed quickly, PKU can result in stunted growth, microcephaly, and brain damage. In the early 1970s Mitchell was at the New England Newborn Screening Program when Jean Dussault, a Canadian physician who became a close personal friend, realized that the approach to early detection of PKU could be applied to congenital hypothyroidism. The disease had frustrated doctors for years because of the knowledge that early detection and treatment could head off symptoms before, to use Mitchell’s word, they “blossomed.” Congenital hypothyroidism was added to the screening protocol later that decade.
In the early days of testing in Quebec, around 1972, says Mitchell, “when Dussault would get a low value or an abnormal value, they didn’t have a network established to identify who these families were, so they had to send nurses out into the field to find them.” Computerization was limited to data entry on punch cards. Part of what Mitchell did in Massachusetts was to establish systems for collecting, analyzing, and following up on blood samples. “We would notify the pediatricians, saying, ‘You’ve got an infant who has congenital hypothyroidism, so get on the ball and get her in,’” he recalls. Originally the incidence of the disease was thought to be about one in 4,000, but as testing has become more regular researchers are finding that it is more common.
The phone call to Stout’s parents in 1991 is now part of Stout family lore. Her pediatrician, alerted by Mitchell’s lab, conveyed the diagnosis to Stout’s parents just a few days after they took her home.
“My mom was freaking out all weekend; she had no way to look up all the stuff you can get off the Internet nowadays,” says Stout. There was some comfort in the doctor’s words. “He kind of explained what it was and that as long as I got to an endocrinologist right away on Monday everything would be fine.”
Stout’s family followed doctor’s orders. And she got her first dose of a hormone that she has been taking every day since. Now it is in the form of “a little pink pill, and it actually tastes pretty good,” Stout says. Her treatment hasn’t changed since she was a baby other than that her dosage went up as she grew. Her long-term prognosis is good as long as she keeps taking the medicine.
Growing up in Westborough, Massachusetts, Stout was captain of the ski team in high school. She was an avid racer and went to the state championships. Music has always been a big part of her life. She plays the violin and the viola and was a music minor and biology major in college. During her time at Mount Holyoke she also was president of Best Buddies, a group that put her in direct contact with developmentally and cognitively impaired students at the Berkshire Hills Music Academy in South Hadley. She also joined the Medical Emergency Response Team on campus and was trained as an emergency medical technician.
Today Stout works as a research assistant in gastrointestinal immunology at the Boston Children’s Hospital (BCH) and has her sights set on medical school. She developed an interest in pediatric endocrinology during high school when she and her mother were on a panel, organized by the BCH, aimed at teaching parents of younger children with hypothyroidism what it is like to grow up with the condition.
“It’s kind of amazing to think of what they can do and a little scary to think of what would have happened if they didn’t do it,” Stout says.
Mitchell contacted Stout early last year to see if she would give a short speech, sharing personal testimony on the benefits of newborn screening. She agreed. “Madeleine was obviously ideal.
A college graduate, she was now working in the medical field and she is articulate,” said Mitchell.
Stout said that speaking at the State House was “a little intimidating” because of the cameras and the high-level officials who followed her at the podium. “They kept telling me I was pretty much the most important person there because I gave a face to newborn screening; instead of just telling what a great thing it is, I was living proof that it changes lives.”
Today, UPS trucks visitevery hospital and birthing center in New England every afternoon to collect dried drops of blood from babies born in the region, which can number from a few hundred to more than a thousand, explains Roger Eaton, the current director of the newborn screening lab. The samples arrive at the lab the next day, and technicians perform tests that screen for thirty-one different conditions. The advent of tandem mass spectrometry in the 1990s expanded the number of detectable congenital metabolic diseases. “The next morning the computer will give us a list of the specimens that we should be concerned about,” said Eaton. Then the work of contacting physicians and possibly doing follow-up tests begins.
“Thankfully, almost every baby born is in fact fine, and they never hear from us,” says Eaton. There are also those that have obvious “clinical manifestations” of disease. The cases that interest him most are those where, “Even an astute physician would say, ‘Congratulations you have a beautiful baby with ten fingers and ten toes,’” he says. “The condition Madeleine has is a very good example of that.”
Dr. Richard Olney, a medical officer with the Centers for Disease Control and Prevention in Atlanta who tracks newborn screening programs around the country, says the number of tests conducted during the first hours and days of life “has exploded in the last ten years.” The approximately four million babies born in the United States each year are tested for maladies that fall into several broad categories such as metabolic conditions (PKU and galactosemia), endocrine conditions (congenital hypothyroidism and adrenal hyperplasia), and blood conditions (sickle cell disease) as well as other congenital conditions such as cystic fibrosis.
“Hospitals have always done things with newborns to keep them healthy, like giving them vitamin K and putting drops in their eyes so they don’t get infections,” says Olney. “There has been a push in the last ten years to try to make screening more uniform across the country.”
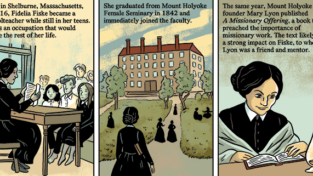
 These so-called “point of care” screenings go back to the Apgar score developed in 1952 by Virginia Apgar, a 1929 graduate of Mount Holyoke who blazed trails in medicine. The Apgar score is a visual assessment of a newborn’s well-being that rates a baby on the basis of its complexion, pulse, reflexes, activity, and respiratory effort.
These so-called “point of care” screenings go back to the Apgar score developed in 1952 by Virginia Apgar, a 1929 graduate of Mount Holyoke who blazed trails in medicine. The Apgar score is a visual assessment of a newborn’s well-being that rates a baby on the basis of its complexion, pulse, reflexes, activity, and respiratory effort.
The Apgar score is a prime example of a practice that, Olney says, has become a “standard of care,” which is his goal for newer screenings that test hearing and look for heart defects (using pulse oximetry). Of the thirty-one tests currently recommended as part of newborn screening, twenty-nine are blood-based, he says.
The State House’s recent recognition of fifty years of newborn screening was a welcome celebration of progress and achievement for those in the field. “It was nice to have a spotlight on the work we do day after day behind the scenes,” said Eaton.
But speeches and political proclamations aside, the most gratifying recognition for the technicians and medical professionals who devote their lives to the task of faithfully processing and screening millions of tiny blood droplets is to see the human impact.
When he was director, says Mitchell, “occasionally we had a grateful mother come through with her baby and go through the lab showing everyone what they had done. . . . You can talk about monetary rewards, but it doesn’t compare with this, it really doesn’t.”
Meeting Stout last November was special. Mitchell says, “We don’t get to see the live baby in the lab. So here, suddenly appearing in front of us, was this mature young girl, articulate, lovely, bright, and you say to yourself, ‘Oh my Lord,’ I looked at her lab values, and she would have been brain damaged if her blood spot hadn’t gone through our laboratory. . . . Now here she is. Just the personification of a young woman you would love to have as your daughter. You can’t help but be thrilled; it’s marvelous.”
Stout doesn’t feel like her disease defines her, but she is glad to lend her face and her voice to efforts to explain and promote the benefits of newborn screening for conditions like hers. “If they ask me again, I’ll of course say yes,” she says.
—By Eric Goldscheider
Eric Goldscheider (eric.goldscheider@gmail.com) is a freelance writer based in Massachusetts.
—Illustrations by Alex Nabaum
This article appeared in the summer 2014 issue of the Alumnae Quarterly.
July 14, 2014










Leave a Reply